I get a lot of questions from practitioners about clients who have gallstones, cholecystitis (inflammation of the gallbladder), or who have already had their gallbladder removed.
What special considerations are needed to manage these types of issues?
Well first, let me just say that I feel there is a lot of unnecessary gallbladder surgery.
Yes, you can survive without your gallbladder, just like you can survive without your tonsils and your appendix, but I think it’s important to have your gallbladder if at all possible. I always look at what interventions are possible outside of surgery.
In particular, a lot of people have surgery as a result of a gallstone attack, which can be painful, but are often fairly harmless if treated. When people are doubled over in pain they go to the hospital or doctor and the doctor immediately wants to cut out their gallbladder. Not to say that all gallbladder surgery is unnecessary, but a lot of gallbladder surgery is unnecessary.
I have a lot of suggestions relating to how to help your client during a gallstone attack, as well as how to help them after gallbladder surgery should they go that route, but first let me talk a bit about the gallbladder and what is going on when a client is having problems in the first place.
What functions does your gallbladder perform?
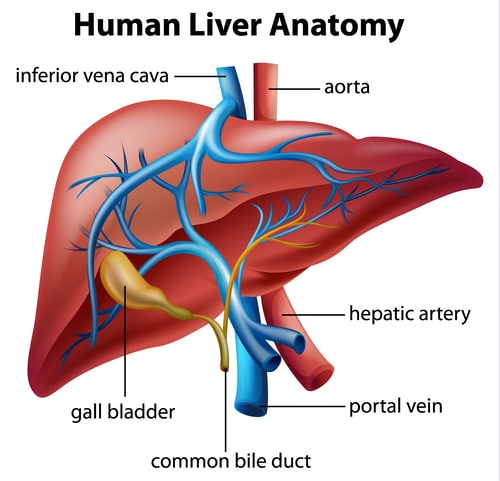
Your liver produces bile and the bile gets concentrated in the gallbladder and stored there. When you eat a fatty meal the bile gets released from the gallbladder and starts to break down the fats into little tiny globules. Then lipase that is secreted from the pancreas mixes in with the tiny globules and bile, emulsifying the fats.
The gallbladder also secretes bicarbonate that mixes with the bile (as it goes into the duodenum) and alkalizes the food that has become acidic from the stomach. The bile goes from a pH of 2.2 to about a pH of 8 in the duodenum. This alkaline environment is needed to begin starchy food digestion with the amylase enzyme that the pancreas secretes.
So to summarize, your gallbladder:
- Stores and concentrates bile
- Secretes bile when needed to break down fats
- Secretes bicarbonate into the small intestine creating an alkaline environment needed for starchy food digestion.
What causes gallbladder problems?
People experience a few different issues relating to their gallbladder, the most common being the formation of gallstones. Gallstones occur when cholesterol and other substances found in the bile form solid stones. These stones can be small or large, and many times go completely unnoticed. It is estimated that 20% of the adult population in the U.S. have stones, but only 1-3% of those actually experience any symptoms.
The problem occurs if the stone passes from the gallbladder into the small intestine or becomes stuck in a bile duct, both of which can cause pain. Inflammation and even infection can then occur.
There are a number of things that can lead to gallbladder issues:
- Food allergies (especially eggs, wheat, coffee, pork, and onions). Eating allergy-causing foods stimulates the swelling of the bile ducts. The swelling reduces the flow of bile from the gallbladder, and causes the pain and other symptoms connected with a gallbladder attack. Caffeine, especially, such as in coffee, can stress out the gallbladder.
- Inadequate stomach acid
- Lack of exercise
- Weight fluctuation: A large weight gain or even a rapid weight loss. When you have a rapid weight loss, you have a lot of toxicity that the liver is dealing with, so the bile tends to get thick and sluggish.
- Childbirth: Frequency increases risk.
- Birth control pills or synthetic hormones: Females are more prone to get gallbladder disease than males because of the effects of estrogen and birth control pills. Estrogen dominance has a huge impact on the health of the gallbladder. Considering that estrogen and the mineral copper closely parallel one another, many women have copper toxicity problems due to estrogen dominance, and then gallbladder problems because some of those bile salts are copper salts – that’s where the bile gets its green color from – copper! You don’t have to be on The Pill or taking hormones to have a gallbladder problem related to your hormones – it can be from inefficient hormonal detoxification. Guys, too – you can have testosterone and estrogen problems.
- NSAIDs: and other anti-inflammatories can take their toll on the liver and gallbladder. Other medications can, too, but NSAIDs more often, especially for chronic users.
- Smoking
- Alcohol: This is individualized, but obviously too much alcohol is not healthy for your liver, gallbladder, or the rest of your body
- Constipation: Makes the bile really thick and sludgy, which causes gallbladder issues like
gallstones.
- Excess refined and artificial sugars in the diet: Aspartame (Nutrasweet) and other excitotoxins (MSG)
- Refined carbohydrates – these, along with the bad fats, are where the oxidation (free radical damage) and the inflammation comes from, and it can take its toll on the gallbladder because of its effect on cholesterol
- Bad fats – these include the obvious partially hydrogenated “trans” fats, but also those refined polyunsaturated vegetable oils that so many think are good to eat – corn, soy, canola, safflower, sunflower, peanut, cottonseed, and grapeseed
- Parasites
- Hispanics, Native Americans, and Caucasians of Northern European descent are most likely to be at risk for gallstones.
- Heredity: If you have first degree relatives who have had gallbladder issues you are more likely to have them as well.
How can you help clients prevent and heal gallbladder issues?
If your client is feeling right shoulder pain, or feeling a pain under their right rib-cage, they may have a liver/gallbladder problem brewing.
If you test your client and they have high cholesterol, high LDLs, low HDLs, a little bit high or even a lot high on alkaline phosphatase; GGT, LDH, SGOT, and then they also have a uric acid that’s decreased, that would be a good sign that there is liver/gallbladder stress. They don’t have to have all of these, just a few.
So how can you help that client? Or what advice can you provide to prevent issues in the first place?
First, here are some diet and lifestyle recommendations to protect and heal the gallbladder:
- Breathe and relax before eating
- Chew thoroughly
- Avoid sugar, refined carbohydrates, gluten, and alcohol
- Avoid trans and bad fats
- Identify and eliminate food allergies
- Eat essential fatty-acid-rich foods (chia, flax, hemp, and pumpkin seeds)
- Eat chlorophyll-rich foods (as well as bitter greens which stimulate the bile)
- Drink lots of water
- Don’t overeat – it overtaxes your fatty metabolism
- Don’t skip meals – it causes buildup of bile
- Regular cleansing – give yourself a break from heavy-duty foods; try green juices, green smoothies, greens, and bitters.
Supplements that support your liver/gallbladder:
- Bitters to stimulate bile production
- Lipase
- Taurine
- Vitamin C
- Liver cleansing herbs: milk thistle, dandelion, yellow dock, and burdock root
- Liver stimulating herbs: fennel, anise, and cayenne
- Lemons and beets: great foods for your liver and gallbladder – they help to keep bile healthy and non-viscous
- Lecithin
- Peppermint oil
- B vitamins
What if my client is having a gallstone attack?
First, I am not suggesting that you treat a gallbladder problem on your own. It’s really a good idea to have a practitioner on board that has the right knowledge to guide you. For example, it’s important to do ultrasounds to diagnose the size and location of gallstones.
But there are some things you can recommend if a client is experiencing an attack but doesn’t want to go to the hospital for surgery.
- Fasting can be very helpful especially if your client is in an acute stage. Have them fast and sip lemon water slowly so that the duct doesn’t go into spasm and cause a blockage. Take one-half of a fresh squeezed lemon and mix it with about 6 oz of water and sip it (don’t gulp it down) over the next 30 minutes
- Juicing
- Fermented beets – thins the bile
- Foods and herbs that thin the bile: turmeric, milk thistle, artichoke, and dandelion
- Apple Cider Vinegar – contains malic acid, which softens the bile.
- Anti-inflammatory herbs – turmeric, ginger, boswellia, and quercetin. Ginger also helps with the nausea.
- Antispasmodic herbs – valerian and chamomile
- Cold pack – You can also try a cold pack over the area of your gallbladder – the upper right quadrant of your abdomen. Place the cold pack about half way over your ribs and half over the abdomen. Make sure it is wrapped in a towel, and not directly on the skin. This should give some relief to the heat the spasms create.
How can you manage a client post gallbladder removal?
As I said earlier, a person can live without a gallbladder, but it is important to realize the digestive/elimination functions that they won’t have naturally happening without a gallbladder. You need to help them address these functions through diet and supplements.
There are a couple of things that happen when your gallbladder gets removed: you no longer concentrate the bile so you are not very efficient and effective at breaking down fats. You also don’t neutralize the food bolus from the stomach effectively, so you have inefficient absorption of carbohydrates. And then, finally, you don’t have that alkaline secretion to help keep the digestive lining nice and healthy.
When you work with your client, here is a list of special considerations that need to be implemented. Your client needs to:
- Avoid fried foods and trans fats.
- Minimize or avoid dairy.
- Avoid fats cooked with sugar.
- Reduce grains (since they now have an inefficient digestion of starch without the gallbladder’s bicarbonate).
- User bitters before meals (to stimulate bile production and movement).
- Supplement with lipase (fat digesting enzyme).
- Supplement with bile salts (helps your body emulsify the fats; 2 with all fatty meals, 5 days on, 2 days off, until feeling well; cycle on and off).
- Avoid late night snacking (letting the body heal and detox).
- Add hemp seeds, chia seeds, algae, flax, walnuts; the essential fats.
- More protein – to repair the stomach lining (supplement with protein powder, green powder, or spirulina powder if you need to).
Learn more about what I teach my practitioners about the digestive functions, along with other body and endocrine systems, in my Nutritional Endocrinology Practitioner Training program. Discover the curriculum modules and other aspects of the program. Enrollment is by application only, and you can apply at this link – http://www.NEPTApply.com. After you apply, you’ll be directed to schedule a time to speak with us and have your questions answered.
Share this:
Are you feeling stuck?
Do you feel as if something is missing from your practice that's keeping you from delivering breakthrough outcomes for your clients?.
Recent Posts
Our Programs
Nutritional Endocrinology Practitioner Training (NEPT)
The Mastery and Certification tier is our flagship program and provides everything you need to feel confident as a practitioner who knows how to get results that lead to healthy and happy clients.
Functional Assessment Mastery
Explore the relationships between the most important hormones and their relationship with nutrition.
Functional Nutrition Mastery
Learn how to support your clients to eat and supplement in a way that reduces and eliminates chronic symptoms.
Medical Disclaimer: The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Ritamarie Loscalzo, drritamarie.com, and the experts who have contributed. We encourage you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
Disclosure: Sometimes (but not always), when I share resources in my programs, newsletter, and on my website, I'm using an affiliate link, which means I do make money if you buy. My credibility is extremely important to me; therefore, I only endorse the products, services, and people I believe in. DrRitamarie.com is independently owned and the opinions expressed here are my own.
Click here to see our Privacy Policy.




 gallstones.
gallstones.









I was delighted with the excellent advice in your article! I had shingles 5 months ago and at the same time had agonizing pain in the gall bladder/liver region.
The Specialist said I needed to have my gall bladder removed. However I always get copies of test results and knew there was no gall stones, so questioned my GP. He sent me to another Specialist who reviewed the same test results and concluded that there was no evidence that I needed my gall bladder removed. He said wait and do another ultrasound in a few weeks. The CBD went from 12cm to 10cm. He said it will probably come down more and scheduled another ultrasound later in the year just be to certain.
I did do a ‘liver/gall bladder detox’ before the second ultrasound and this really seemed to help reduce the pain. It was a really good quality highly regarded one and very gentle, easy and pleasant to do.
I also discovered that the pain was a referred pain coming from the shingles. How can I be sure? Because, as the shingles improved the ‘gall bladder’ pain improved at the same rate. So I am quite confident that the two were linked (as my Naturopath suspected). I am not the only one I know of who has had liver/gall bladder pain when getting the shingles and it turned out to be referred pain.
Imagine, wrong diagnosis, and still pain after surgery? I’d have added to my pain, not reduced it!
By the way that first “Specialist” said that removal of my gall bladder wouldn’t make any difference to my digestion and I’d still be able to eat everything as usual – ??? It made a big difference to my Dad after he had GB surgery! I have multiple food allergies so was not willing to risk losing any valuable body part without a fight!
Happily, I still have my gall bladder but no more pain!
Thanks again for your fabulous article and advice!
Hi, Nola, I’m so happy to hear that you trusted yourself to not have your gall bladder removed, and to get another opinion. Hopefully there will be some helpful tips in our article that will help you in the future. If there is anything else we can do to be of help, always feel free to reach out to us.
Lynn DeBuhr Johnson
Dr. Ritamarie Programs
Institute of Nutritional Endocrinology
Hello! Thank you for your excellent information.
Quite amazing to receive this one concerning gallbladder/liver today!! Pain excruciating and after U/S and X-rays last week was told no stones but now still in pain. Doctors gave no dietary advice at all.
So I am very grateful for your advice. I’m allergic to lemons, is there anything else I could sip?
I muscle test everything and my body doesn’t want apple cider vinegar or grapefruit juice at the moment. (Doctor did say my stomach was over acidic.)
I understand you’re unable to give help like this but I would appreciate a substitute for the lemon to soothe pain. I have it under right rib cage to kidney/adrenal at the back.
Do you do consultation on-line and what is the cost please.
Thanks again for you help. I’m planning to get your cheesemaking offer asap – I also want to make my own nut-milk – store bought always tastes metallic and yes, I don’t trust the packaging 🙂
Best wishes, Julia Olwyn
Hi Julia! Thank you for your comments, and yes I am afraid you would need to be a participant in a program to receive direct replies/advice from Dr. Ritamarie. The most direct help from Dr. Ritamarie is available from our Energy Recharge Coaching program and you can find out more details and the cost from a free strategy session: http://www.ERCApply.com. Or a simple and very cost-effective place to get access to once-a-month coaching calls is through our VITAL Community: http://www.VITALHealthCommunity.com. I hope this gives you some great places to start. Best wishes! ~ Stacey Terry, Care Team
Hi, Julia, Along wit Stacey’s excellent advice, I’d also encourage you to fill out a Health Consultation Request form for a complementary consultation with us to see other ways we might be of help – https://drritamarie.com/wp-clone/faq/nutrition
Also, you might also consider starting the day with a glass of fresh celery juice, if you can’t do the lemon or apple cider vinegar.
Lynn DeBuhr Johnson
Dr. Ritamarie Programs
Institute of Nutritional Endocrinology
I had no idea the attacks I was having was from gallbladder attacks until I had one I could not breathe or function through. I went to the ER and after CT scan and ultrasound I found out my gallbladder was infected and inflamed and needed to be removed . This was a week ago and I remember being very upset the next day thinking maybe there was another option. I get that feeling all over again when I read articles like this because everyone has an opinion. I was my told in my case it was necessary because of the infection so that I would not risk the infection spreading to my other organs. Are you saying that I didn’t have to get it removed after all?
Hi, Michelle. Thank you for sharing your experience. It was never our intent to share any information that would have you doubt the recommendations of your medical provider.
However, since you have had your gallbladder removed, I encourage you to read the section of this article on what you can do after you’ve had your gallbladder removed. There are many things you can do to continue to have a healthy body.
I have just spent a week in hospital and after ultra sound and an MRI scan I was tol I had sludge in my Gall Bladder and need surgery to remove my gall bladder but I refused, is there a method to remove the sludge.???
Hi Raphael, what is the sludge, and how are you doing now? You can join Dr. Ritamarie’s Unstoppable Health Facebook Group to get some more support there. https://www.facebook.com/groups/UnstoppableHealth/ Wishing you health in the new year Raphael.