HOME > reinvent healthcare podcast > A Functional Approach to Hormonal Balance Assessment
A Functional Approach to Hormonal Balance Assessment
By Ritamarie Loscalzo

In the complex human body, achieving and sustaining hormonal balance is critical for ensuring optimal health. Even minor disruptions can have significant effects on well-being. Therefore, a comprehensive understanding of the factors influencing hormonal homeostasis and the tools for accurate assessment becomes paramount.
A Deep Dive into Factors Disrupting Hormonal Balance
The body’s intricate web of hormones is susceptible to a lot of disruptive influences. Just one change in the hormone web can throw the hormonal system into disarray, leading to a cascade of downstream effects impacting a client’s overall health. Here, we dive deeper into these well-defined factors to better equip you with a comprehensive understanding of hormone balance and influence.
Chronic Stress
The stress response, a primal survival mechanism mediated by the release of cortisol from the adrenal glands, is essential for navigating acute challenges. However, in today’s fast-paced world, chronic stress becomes persistent and leads to hormonal imbalances. Chronically elevated cortisol disrupts the delicate feedback loops governing hormone production.
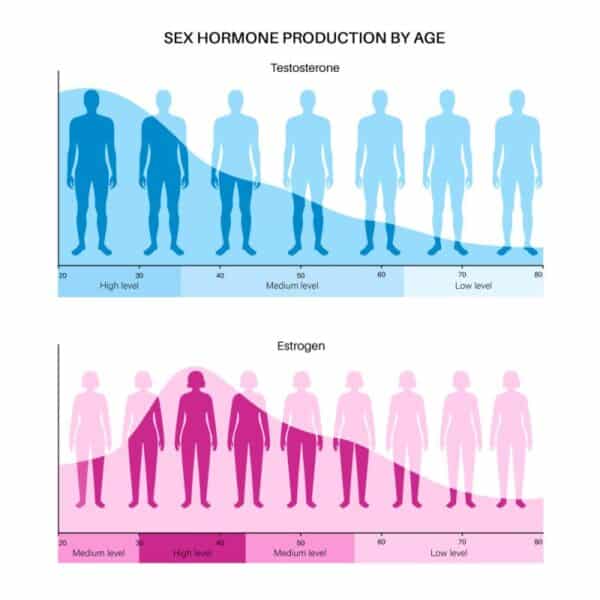
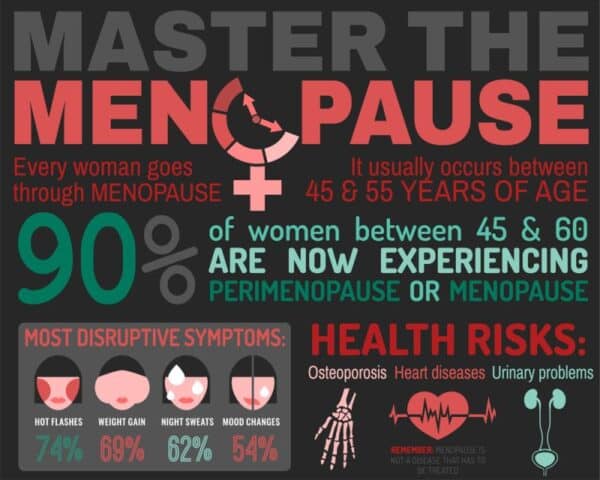
Sex hormone production, which also involves the adrenals and is essential for reproductive health and libido, can be significantly dampened. Thyroid function can also be compromised by chronic stress, leading to symptoms of fatigue, weight changes, and mood disturbances.
Dietary Insults
The modern diet, often filled with processed foods, refined sugars, and unhealthy fats, acts as a dietary insult to the hormonal system. These choices contribute to insulin resistance, a condition where the body struggles to utilize the sugar (glucose) from food for energy. This not only disrupts blood sugar control but also creates a chronic inflammatory state and hormonal imbalance. Furthermore, the refined carbohydrates and unhealthy fats often found in processed foods hinder the absorption of essential nutrients that play a role in hormone production and metabolism.
Insufficient Physical Activity
A sedentary lifestyle also leads to hormone imbalances. Regular exercise is a potent modulator of hormonal health. Physical activity promotes healthy insulin sensitivity, helping to counteract the detrimental effects of a poor diet. Exercise also functions as a natural stress reliever, helping to mitigate the disruptive effects of cortisol on other hormones. Moreover, physical activity can enhance sex hormone function, contributing to increased energy levels, libido, and overall well-being.
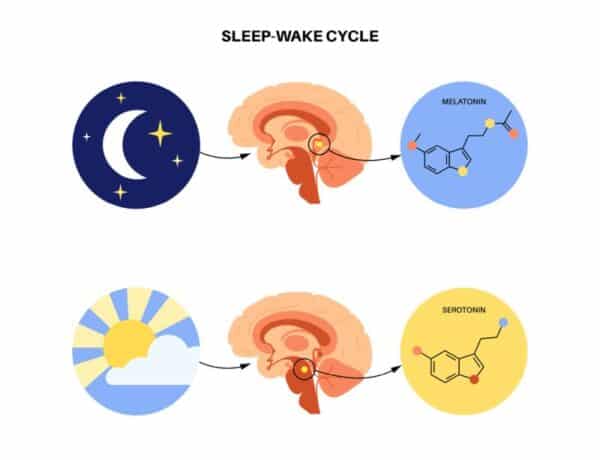
Sleep Deprivation
Chronic sleep disturbances disrupt the release of critical hormones essential for maintaining hormonal homeostasis. Melatonin, often dubbed the “sleep hormone,” plays a key role in regulating sleep-wake cycles. Insufficient sleep disrupts melatonin production, leading to difficulty falling asleep and staying asleep. Growth hormone, another critical hormone released during sleep, is essential for tissue repair and regeneration. Chronically inadequate sleep hinders the production of growth hormones, impacting recovery from exercise and potentially contributing to age-related decline as well as more hormone imbalance.
Genetic Predispositions
Genetics plays a role in determining an individual’s hormonal efficiency. Certain genes can influence the body’s ability to produce, regulate, and utilize hormones. A family history of conditions such as polycystic ovary syndrome (PCOS), diabetes, or thyroid disease can indicate a predisposition to hormonal imbalances. Understanding a client’s genetic background can be a valuable tool for identifying potential hormonal vulnerabilities.
Environmental Toxins
Endocrine-disrupting chemicals (EDCs) are a growing concern in modern healthcare. These environmental toxins, found in pesticides, herbicides, and certain plastics, can mimic or interfere with the action of hormones in the body, leading to hormone imbalance. For example, some EDCs can have an estrogen-like effect, potentially disrupting the menstrual cycle and creating irregular periods and fertility. By understanding the potential impact of EDCs, practitioners can guide clients toward strategies for minimizing exposure and mitigating their disruptive effects on hormonal balance.
By recognizing these factors and their influence on hormonal health, we are able to create a more harmonious hormonal state for clients. In future installments, we will explore strategies for effectively addressing hormonal imbalances and restoring optimal hormonal function.
Assessment Strategies: Tuning into Hormones Through Diverse Instruments
Once a suspicion of hormonal imbalance arises, selecting the appropriate assessment tools becomes a critical step in guiding effective client care. We have a unique advantage in this regard, possessing a diverse toolbox for evaluating hormonal imbalance and health. Let’s take a look at potential assessment strategies, highlighting their strengths and applications.
Blood Tests: The Established Standard
Blood tests are the cornerstone, especially in conventional medicine, of hormonal evaluation, offering a time-tested and reliable method for quantifying certain, but not all, hormone levels. A comprehensive blood panel can assess a broad spectrum of hormones, including:
-
Thyroid hormones (TSH, T4, T3, Free T4, Free T3): These hormones regulate metabolism, energy levels, and mood. Abnormalities in thyroid function or in converting thyroid hormones can have a significant impact on overall health, including the balance of sex hormones, adrenal hormones, and blood sugar regulation. A comprehensive thyroid panel is needed to fully assess not just the function of the thyroid gland itself but also the cell receptors, the conversion from inactive to active, and more. Thyroid hormones are best tested in the blood.
-
Sex hormones (estradiol, progesterone, testosterone, and DHEA): These hormones play a crucial role in reproductive health, sexual function, and bone density. Imbalances in sex hormones can manifest as menstrual irregularities, infertility, decreased libido, and mood swings. There are many downsides to testing these hormones in the blood. One is the lack of differentiation between free and active hormones. In addition, the blood is unable to evaluate hormone metabolites.
-
Cortisol: This hormone, often referred to as the “stress hormone,” plays a vital role in the body’s stress response. Measuring cortisol levels can provide insights into a client’s stress burden and its potential impact on other hormonal systems. Blood tests are of limited usefulness because they only capture a single time of the day, and cortisol varies throughout the day. The testing methods mentioned below are more clinically relevant than blood. For a deep dive into hormone metabolite testing, listen to “Metabolite Testing: Finding the Missing Link in Your Hormone Health.“.
-
Other hormones: Depending on the specific clinical picture, additional hormones such as insulin and growth hormone may also be evaluated through blood tests. Insulin is rarely tested, except in diabetics, and that’s a big mistake. I believe that it should be tested as a routine part of everyone’s annual blood test, as insulin elevation and subsequent insulin resistance can lead to all of our major debilitating diseases, including cardiovascular disease and cancer.
While blood tests offer a wealth of information, it’s important to acknowledge limitations. Blood levels may not always reflect the amount of “free” hormone readily available to tissues. Additionally, certain factors, like blood draw timing and medications, can influence blood test results.
Salivary Testing: A Window into “Free” Hormone Levels
Salivary testing offers a valuable alternative for assessing certain hormones. Saliva reflects the “free” fraction of hormones, unbound to proteins in the bloodstream, and is potentially more indicative of bioavailable hormone levels at the tissue level. Salivary testing is often used for hormone tests.
-
Cortisol: Saliva testing can provide a more comprehensive picture of cortisol activity throughout the day compared to a single blood draw, which may only capture a snapshot in time.
-
Sex hormones: Similar to cortisol, salivary testing can offer insights into “free” sex hormone levels, potentially providing a more accurate reflection of hormonal activity at the cellular level.
However, salivary testing also has limitations. Standardization of hormone tests used across laboratories can be an issue, and factors like salivary flow rate and contamination can impact test results.
Urine Testing: Unveiling the Story of Hormone Breakdown Products
Analysis of urinary hormone metabolites, the breakdown products of hormones excreted in the urine, can provide valuable insights into overall hormonal activity. While not a direct measure of circulating hormone levels, urinary testing can offer a broader picture of hormone production and metabolism over time. This approach is often used to assess:
-
Estrogen dominance: By measuring specific estrogen metabolites in the urine, practitioners can gain insights into estrogen metabolism and potential dominance, a condition associated with various health concerns. While in the blood, you can test the main estrogens, estrone, estradiol, and estrone; in reality, only estrone is usually tested.
The 24-hour dried urine test, however, tests the three main estrogens, E1 (estrone), E2 (estradiol), and E3 (estriol), plus the metabolites 2OH, 4OH, and 16OH estrone and methylated versions as well. This gives a more complete picture of estrogen metabolism, including the risk for hormone-sensitive proliferative diseases, bone health, and detoxification interferences.
Stress is a leading contributor to estrogen imbalance, as detailed in this article about the relationship between adrenal dysfunction and menopause symptoms.
-
Stress hormones: Urinary analysis of cortisol metabolites gives you a more in-depth perspective on the impact of stress, the metabolites related to the stress response, and the impact of chronic stress patterns on other hormones that’s not readily apparent through blood or saliva testing.
It’s important to note that interpreting urinary hormone tests can be complex and requires a comprehensive understanding of hormone metabolism. Additionally, certain medications and dietary factors can influence urinary hormone metabolite levels.
By employing a strategic combination of these assessment tools, functional medicine practitioners can gain a deeper understanding of a client’s hormonal landscape. This multifaceted approach allows for the identification of subtle hormonal imbalances and the creation of personalized plans for restoring hormonal harmony and optimizing overall health.
Why Hormonal Balance Matters
By understanding the factors that disrupt hormonal balance and using a variety of assessment tools, you, as a healthcare practitioner can effectively identify hormonal imbalances in your clients. Equipped with this knowledge, you can then create individualized plans that address the root causes of hormone imbalances and help our clients achieve a state of optimal hormonal harmony.
Personally, the test I use the most is the dried urine test, specifically the DUTCH test. If you’re interested in finding out what is keeping your clients exhausted, overwhelmed, and overweight, Register for my training, Balancing Act: How to Identify The Hormone Imbalances that Keep Your Clients Exhausted, Overwhelmed and Overweight!
Share this:
Are you feeling stuck?
Do you feel as if something is missing from your practice that's keeping you from delivering breakthrough outcomes for your clients?.
Recent Posts
Our Programs
Nutritional Endocrinology Practitioner Training (NEPT)
The Mastery and Certification tier is our flagship program and provides everything you need to feel confident as a practitioner who knows how to get results that lead to healthy and happy clients.
Functional Assessment Mastery
Explore the relationships between the most important hormones and their relationship with nutrition.
Functional Nutrition Mastery
Learn how to support your clients to eat and supplement in a way that reduces and eliminates chronic symptoms.
Medical Disclaimer: The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Ritamarie Loscalzo, drritamarie.com, and the experts who have contributed. We encourage you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
Disclosure: Sometimes (but not always), when I share resources in my programs, newsletter, and on my website, I'm using an affiliate link, which means I do make money if you buy. My credibility is extremely important to me; therefore, I only endorse the products, services, and people I believe in. DrRitamarie.com is independently owned and the opinions expressed here are my own.
Click here to see our Privacy Policy.